According to a study published in the BMJ this week: “On the basis of evidence that gluten may promote inflammation in the absence of celiac disease or non-celiac gluten sensitivity, concern has arisen in the medical community and lay public that gluten may increase the risk of obesity, metabolic syndrome, neuropsychiatric symptoms, and cardiovascular risk among healthy people.
"Patients with celiac disease who develop a myocardial infarction are less likely to have classic cardiac risk factors, such as smoking and dyslipidemia, leading to the hypothesis that the pro-inflammatory effect of gluten exerts an independent cardiac risk.
“As a result, diets that limit gluten intake have gained popularity,” add the authors, noting that NHANES data indicates that “adoption of a gluten-free diet by people without celiac disease rose more than threefold from 2009-10 (prevalence 0.52%) to 2013-14 (prevalence 1.69%),” while consumer survey data suggest that a significant minority of Americans is trying to reduce gluten consumption.
Despite this rising trend in gluten restriction, however, "no long term, prospective studies have assessed the relation of dietary gluten with the risk of chronic conditions such as coronary heart disease in people without celiac disease," observe the authors.
"Thus, using prospective, validated data on dietary intake collected over 20-30 years, we examined the association of estimated long term intake of gluten with the development of incident coronary heart disease (fatal or non-fatal myocardial infarction)."
Avoiding gluten could mean avoiding heart healthy whole grains
Their subsequent analysis of data from 110,000+ men and women over a 26-year period found “no significant association between estimated gluten intake and the risk of subsequent overall coronary heart disease, non-fatal myocardial infarction, and fatal myocardial infarction.”
In fact, those within the highest fifth of gluten intake had a lower incidence of coronary heart disease (277 per 100,000 person years) compared with those in the lowest fifth for gluten intake (352 events per 100,000 person years), said the authors, who speculated that the “avoidance of gluten may result in reduced consumption of beneficial whole grains, which may affect cardiovascular risk.”
As a result, they concluded: “The promotion of gluten-free diets for the purpose of coronary heart disease prevention among asymptomatic people without celiac disease should not be recommended.”
The researchers noted a significant inverse relation between estimated gluten intake and coronary heart disease when they adjusted for refined grain intake, which they said "likely reflects the fact that adjustment for refined grains leaves the remainder of the variance of gluten intake correlated with whole grain intake... Whole grain intake has been found to be inversely associated with coronary heart disease risk and cardiovascular mortality.
"These findings underscore the potential that people who severely restrict gluten intake may also significantly limit their intake of whole grains, which may actually be associated with adverse cardiovascular outcomes."
According to cardiologist Dr William Davis, author of the best-selling book Wheat Belly, eliminating wheat and other gluten-containing grains such as barley and rye can reduce your risk of developing obesity, heart disease, and diabetes; while Dr David Perlmutter, author of best-seller Grain Brain describes grains as “silent killers.”
While some highly refined carbs can cause blood sugar spikes and are often used in foods that contain high levels of salt, sugar and saturated fat; grains or gluten per se are not the enemy, according to Dr David Jacobs, Professor, Epidemiology & Community Health at the University of Minnesota.
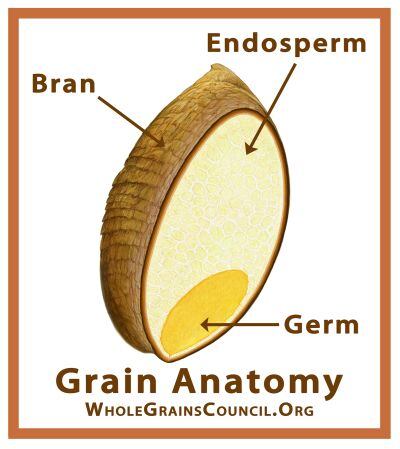
Indeed, whole grains – which contain the bran, germ and endosperm – are associated with better health outcomes, added Dr Jacobs, who was speaking to FoodNavigator-USA at the 2015 Whole Grains Summit: “The evidence is consistent and strong for the beneficial effects of whole grain foods on chronic disease, including cardiovascular disease and other conditions thought to be of inflammatory origin.”
Moreover, a 2012 meta-analysis of 45 prospective cohort studies and 21 randomized-controlled trials (RCT) in the Journal of Nutrition found that people consuming more whole grains were significantly less likely to develop heart disease and type two diabetes, while there was also an inverse relationship between whole grain intake and weight gain, he added.

When it comes to inflammation, meanwhile, whole grains are not the problem, but part of the solution, according to The Whole Grains Council, as they have been shown to reduce markers of inflammation, while observational trials show people who eat more whole grains have a reduced risk of heart disease and diabetes.
Intact whole grains are also low GI foods that provide a steady, slow release of glucose, said Whole Grains Council director of food and nutrition strategies, Cynthia Harriman.
Prospective cohort study
The observational study utilized two cohorts: 64,714 women in the Nurses’ Health Study and 45,303 men in the Health Professionals Follow-up Study without a history of coronary heart disease who completed a food frequency questionnaire in 1986 that was updated every four years through 2010.
Participants were grouped into fifths of estimated gluten consumption (according to energy adjusted grams of gluten per day), and were followed from 1986 until the development of coronary heart disease, death, or the end of the follow-up in 2012.
"The study provides two important conclusions: The intake of gluten is not associated with coronary heart disease and promoting gluten-free diets among people without celiac disease should not be encouraged. That's good news for bakers, and consumers too." Tim O'Connor, president, Wheat Foods Council
* Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA, Everhart JE. The prevalence of celiac disease in the United States. Am J Gastroenterol 2012;107:1538-44, quiz 1537, 1545. doi:10.1038/ajg.2012.219.
Source: British Medical Journal, 2017; 357:j1892, published online ahead of print
‘Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study.’
Authors: Benjamin Lebwohl, Yin Cao, Geng Zong, Frank B Hu, Peter H R Green, Alfred I Neugut, Eric B Rimm, Laura Sampson, Lauren W Dougherty, Edward Giovannucci, Walter C Willett, Qi Sun, Andrew T Chan

"We know that grains are a top source of dietary fiber, one of the most important dietary contributions for heart health, yet nearly 90% of Americans fall short of meeting recommendations for dietary fiber intake.
"Given that gluten-free products oftentimes have low amounts of dietary fiber and lack essential nutrients, of which are found in grain foods, the BMJ findings come as no surprise.
"There is a misconception that a gluten-free diet can bring extra health benefits and weight loss; however, as evidence shows, a gluten-free diet devoid of grains deprives consumers of essential nutrients such as dietary fiber and B vitamins, can cause weight gain from added sugars and fats found in gluten-free products, and ultimately can increase the risk for heart disease, as shown in the BMJ study."
Glenn Gaesser, PhD, Professor of Exercise Science and Health Promotion at Arizona State University and Grain Foods Foundation Scientific Advisory Board Chairman

NON CELIAC GLUTEN SENSITIVITY: While it is estimated that fewer than 1%* of Americans have celiac disease, it is not known how many people have non-celiac gluten sensitivity (they react negatively to some gluten-containing grains, yet celiac disease and wheat allergy have been ruled out), because there are – as yet - no validated biomarkers or diagnostic tests for NCGS.
Some researchers believe people with NCGS may in fact be sensitive to some relatively rapidly fermentable carbohydrates in some gluten-containing products, such as oligofructose and arabinoxylan, and that exclusion of these and other fermentable oligo-, di- and monosaccharides as well as polyols; (also referred to as ‘FODMAPs’) could be the answer to their digestive discomfort.
