The proposal in question involves removing vitamins C and A as mandatory micronutrients and requiring manufacturers to declare Vitamin D and potassium, which are now considered “nutrients of public health significance” along with calcium, based on the 2010 Roadmap to the Dietary Guidelines (read more on the proposed changes here). Marion Nestle, PhD, New York University, took issue with voluntarily adding vitamin D to labels, raising questions about its status as a vitamin and its efficacy when consumed orally.
“’Vitamin’ D is not a vitamin; it is a hormone synthesized by the action of sunlight on skin,” she wrote last week on her blog Food Politics. “For this reason alone, it does not belong on the food label.”
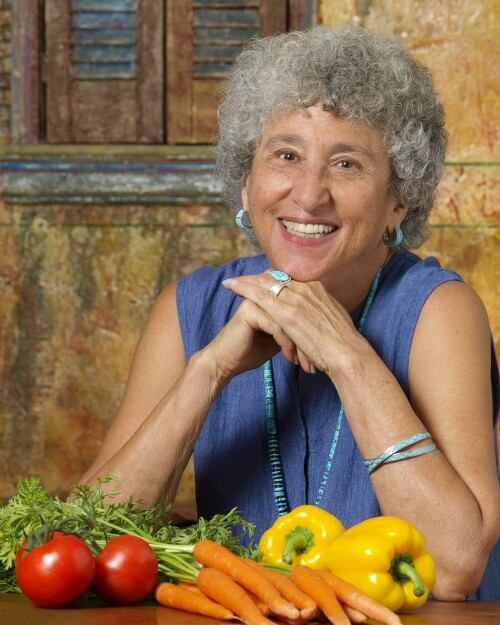
Speaking with FoodNavigator-USA a few days after posting the blog entry, Dr. Nestle said she suspects that proponents of vitamin D supplementation likely pushed to get it added to labels, claiming that using 25-hydroxyvitamin D criterion to measure deficiency is suspect.
“Making the active hormone is a multi-step process, beginning with sunlight on skin,” she said. “It is so much more efficient to obtain the hormone from the action of sunlight on skin and it doesn’t take much skin exposure to meet requirements [15 or 20 minutes produces the equivalent of taking 20,000 IU orally]. Supplements bypass the regulatory controls of the hormone, which is made as needed and stored, or not made if there’s already too much.”
Vitamin D expert Michael Holick, MD, PhD, Boston University Medical Center, said that while he’s “all for sunlight”, he also recognizes the efficacy of orally administered vitamin D—with without the side effects of UV exposure—which is supported by numerous studies (see here, here and here).
“We know a lot about oral vitamin D from a multitude of studies,” he said. “We know that the vitamin D you get from the diet and or fortifying foods is metabolized identically as when you are exposed to sunlight.”
Form, dosage of vitamin D still contested; FDA hasn’t addressed bioactivity of D2, D3
Vitamin D refers to two biologically inactive precursors, D3 and D2. D3, also known as cholescalciferol, is produced in the skin on exposure to UVB radiation. D2, also known as ergocalciferol, is derived from plants and only enters the body through the diet. Both D3 and D2 precursors are transformed in the liver and kidneys into 25-hydroxyvitamin D, the non-active “storage” form, and 1,25-dihydroxyvitamin D, the biologically active form that is tightly controlled.
Many researchers agree that many people are vitamin D deficient and need vitamin D supplements, but the form and recommended dose are still up for debate. Indeed, in recent comments to the FDA on its Nutrition Facts proposals, the Council of Responsible Nutrition called on the agency to take a stance on D2 and D3 by either defining them as bioequivalent or “listing a potency conversion factor if, in fact, the agency considers one form more bioactive than the other.”
Per the Institute of Medicine (which Dr. Holick referenced), serum 25hydroxyvitamin D of 20 nanograms per milliliter are necessary for good bone health. According to the Endocrine Society, between 21 and 29 ng/ml is considered an insufficiency, and 30 and above sufficient in order to maximize bone health and take advantage of the benefits of vitamin D.

Will more fortification lead to overconsumption?
Because the hormone vitamin D is naturally found in very few foods, it’s present in most foods as a result of fortification. Dr. Nestle said that permitting vitamin D disclosure on food labels will likely encourage fortification of foods that may not otherwise be recommended, providing the example of Yum Bunny Caramel Milk Spread, a spread fortified with vitamin D at 10% of the DV that’s “clearly aimed at children” on her blog.
The potential for more vitamin D in the food supply also raises questions about overconsumption and toxicity, as vitamin D is a fat-soluble hormone stored for long periods in body fat, she said. Indeed, the IOM said it is concerned about the possibility of adverse consequences from overconsumption through supplementation or fortification.
But Dr. Holick noted that as long as manufacturers put the amounts they say they are in products, overconsumption isn’t a concern for children or adults. “The IOM says the upper limit in children over 1 is 2,500 units a day and 4,000 a day in adults—but up to 10,000 units is perfectly safe,” he said. “Even if you drink a gallon of milk or fortified orange juice, you couldn’t get anywhere close to those ranges.”
