To put the latter point in perspective, 14.5% of children aged 2-4 years in the WIC program (which provides low-income pregnant, breastfeeding, and postpartum women, infants, and children up to age five with nutritious, supplemental foods) had obesity compared to 8.9% of 2-5 year olds overall.
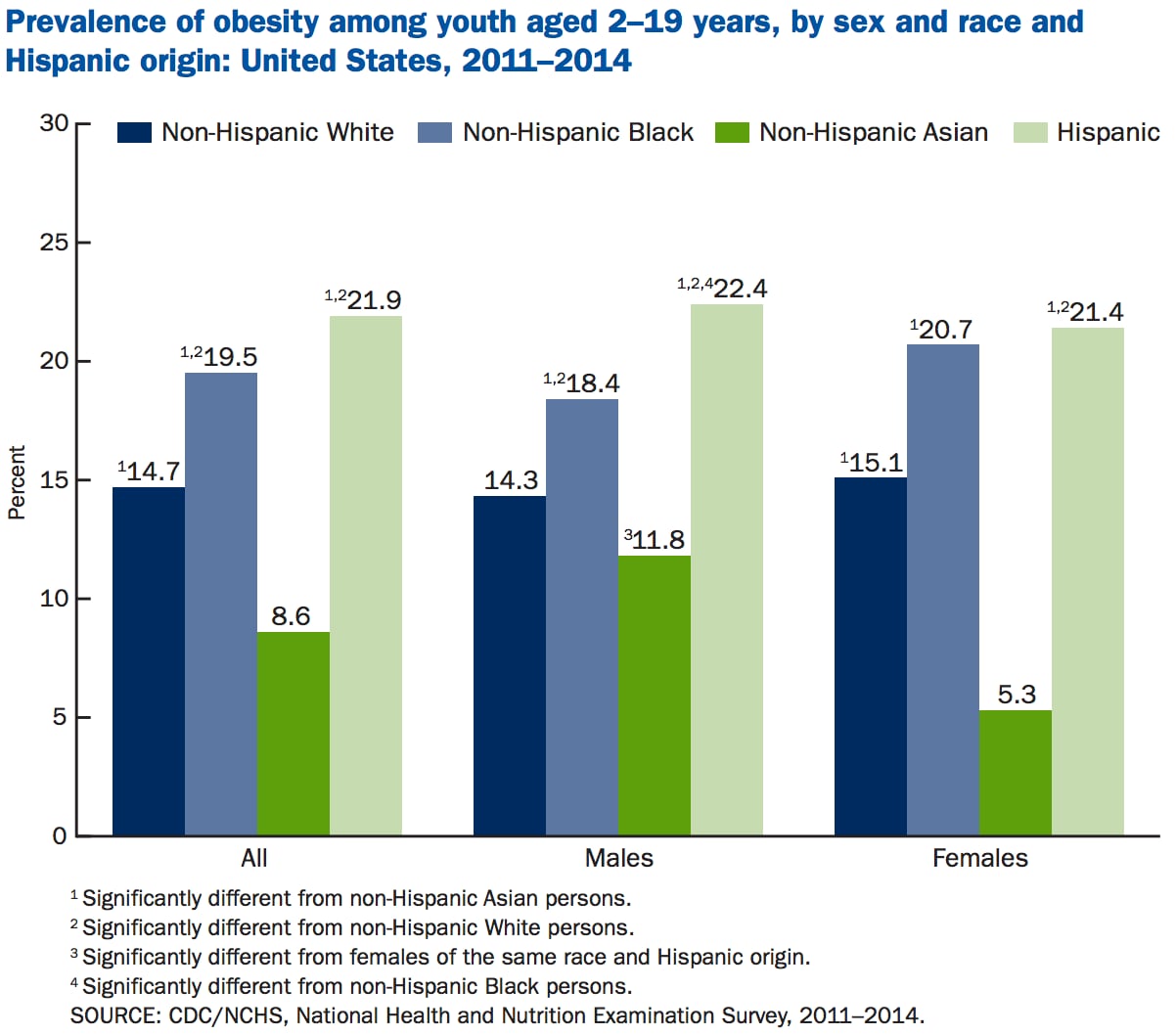
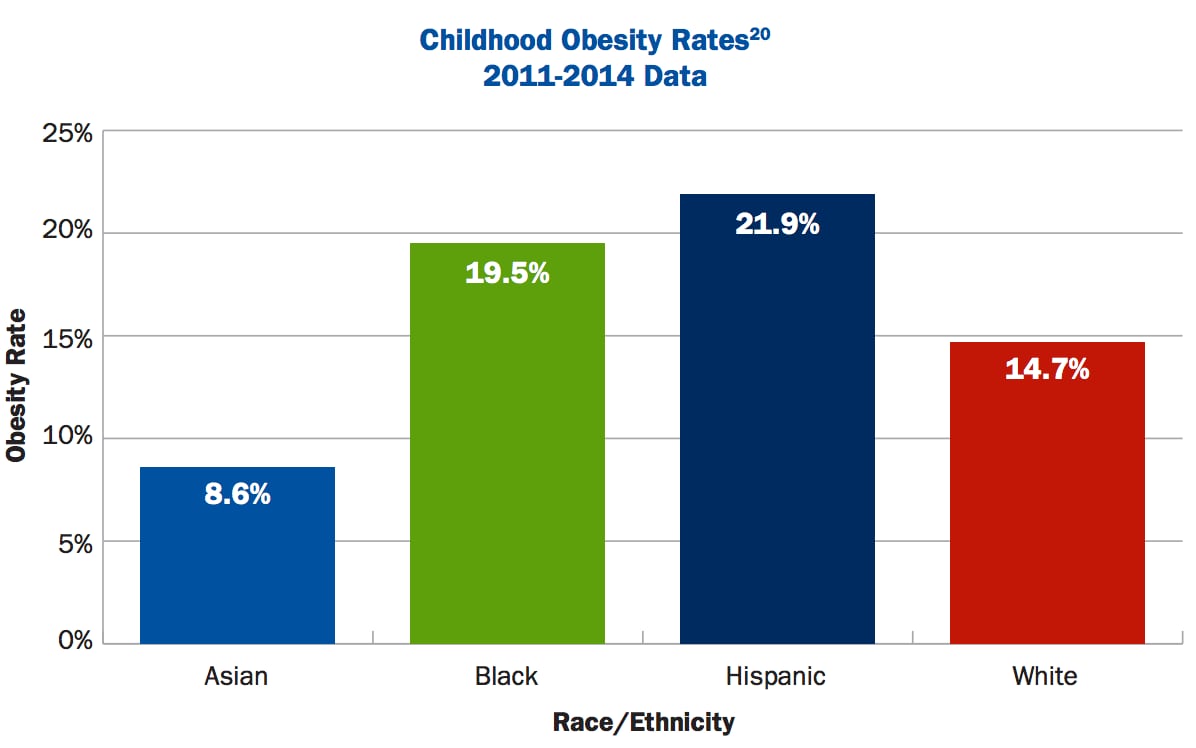
There are also sharp variations in obesity rates between children from different ethnic backgrounds, with the prevalence of obesity far higher among Hispanics (21.9%) and non-Hispanic blacks (19.5%) than non-Hispanic whites (14.7%) and non-Hispanic Asian children (8.6%).
But are things getting better?
FoodNavigator-USA (FNU) caught up with Dr William Dietz (WD), a former director of the Division of Nutrition, Physical Activity, and Obesity at the CDC and currently the director of the Sumner M. Redstone Global Center for Prevention and Wellness at the Milken Institute School of Public Health at George Washington University, to find out...
FNU: Are rates of childhood obesity slowing or declining?
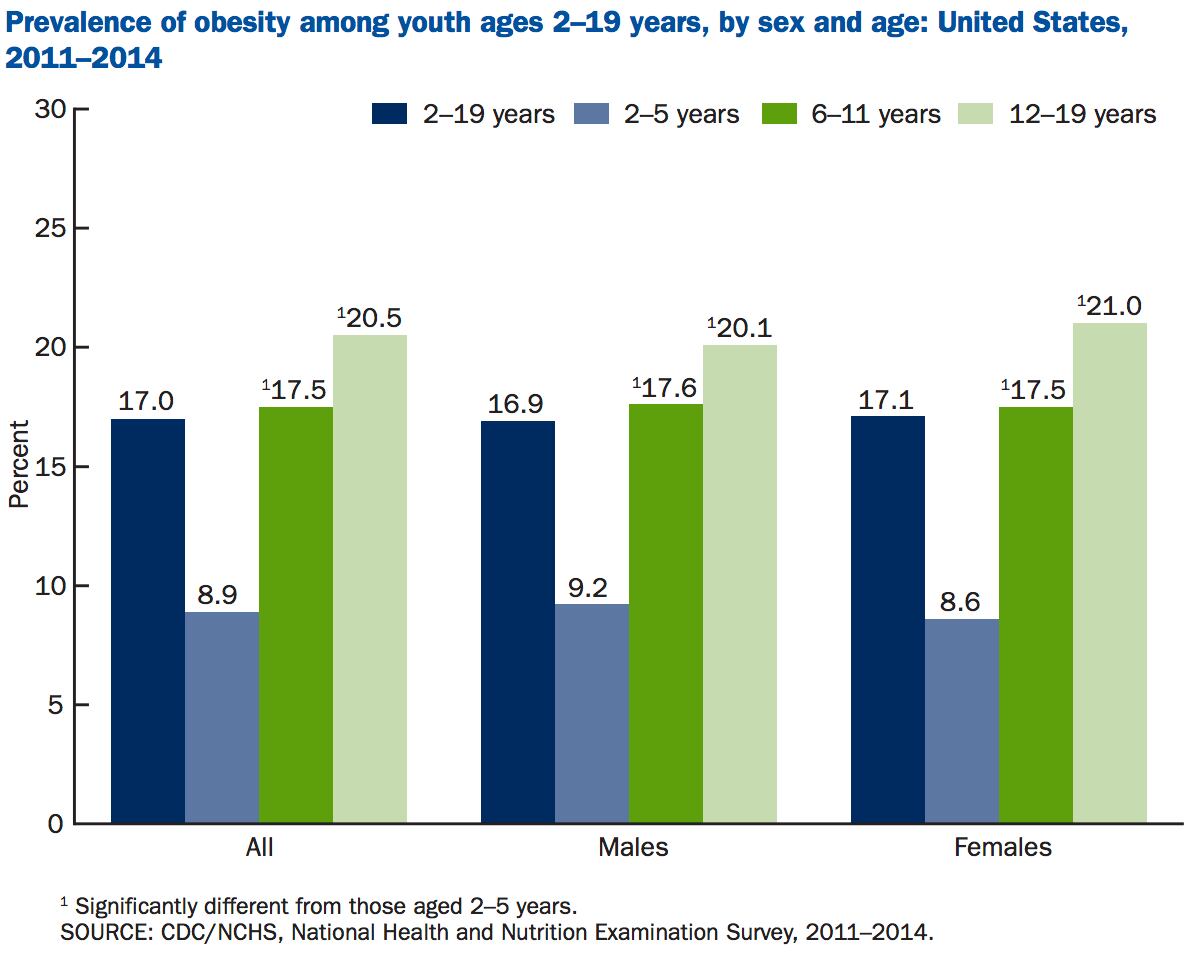
WD: The prevalence of obesity in 2-5 year olds has decreased, and rates in 6-11 year olds are flat, but it’s increasing in 12-19 year olds. We’re also seeing key differences between ethnic groups, so for example, at age 12 the mean BMI of African American girls starts to diverge from that of white girls and that feeds into adulthood where there are marked disparities in rates of obesity.
FNU: What do we know about the impact of early feeding behavior?
WD: We know kids that are breastfed for at least 4-6 months are less likely to develop obesity in later life, and rates of breastfeeding have improved, but the problem is duration. When women go back to work after having a baby, it’s really tough. The Affordable Care Act specifies opportunities for lactation support at work sites, but I am not sure to what extent they are actually being implemented, for example.
One of the continuing concerns is early introduction of complementary feeding, because we know that early introduction of solids is one of the factors that promotes obesity.
We also believe that differences between early feeding practices may contribute to the subsequent disparities that arise between ethnic groups, so for example, African American families are more likely introduce early solids and juice drinks before a year of age, although we can’t say with any assurance that it leads to obesity.

FNU: Are kids’ diets getting better?
WD: NHANES [National Health and Nutrition Examination Survey] data shows that children’s calories from fast food, soda and pizza have all decreased over the past decade, which is great, but they’re still consuming way too much.
For example, one in four children in the US has pizza on any given day, and on the days that teenagers eat pizza, our estimates show that they consume about 600 calories from pizza but only compensate for about 350 of those calories, so on the days they had pizza they were likely to overconsume about 250 calories that they didn’t compensate for. The same applies for soda and juice; when you consume those drinks you don’t compensate for the calories.
FNU: Should kids drink juice?
WD: Whole fruit is better option than juice - although low income communities don’t always have the same level of access to fresh fruits and vegetables – and water and low fat milk are best.
I would agree with the American Academy of Pediatrics in recommending no juice for children under the age of one and then advising kids over that age to consume it sparingly, and if they do drink juice, to make it 100% juice.
But there are also other things showing up in the research impacting the choices people make. For example, in the Hispanic community there is a distrust of the local water supply, so we know that in some areas of DC, Hispanic families are spending as much as 20% of their food budget on bottled water just to be safe, even though the DC water supply is pretty good. There is also other research showing this.
FNU: Are you concerned about the decline in liquid milk consumption among children?
It concerns me that intakes are going down as milk is a good source of calcium and vitamin D, especially for girls. Not everyone agrees on this, but if flavored milk is what it takes to get a child to consume milk in school then that’s reasonable.
Between 2010 and 2014, 31 states and three territories reported declines in obesity rates among toddlers (ages 2 to 4) whose families participate in the Special Supplemental Nutrition Program (SNAP) for Women, Infants, and Children (WIC) nutrition program for low-income families.
The national obesity rate among children in the WIC program has also declined from a high of 15.9% in 2010 to 14.5% in 2014, the most recent year for which data are available.
Source: Pan L, Freedman DS, Sharma AJ, et al. Trends in obesity among participants aged 2-4 years in the Special Supplemental Nutrition Program for Women, Infants, and Children— United States, 2000-2014. MMWR Morb Mortal Wkly Rep 2016;65:1256-1260.
FNU: Is the food industry doing enough?
WD: Of course they should do more, but they are taking some action. For example, the 16 food and beverage companies acting together as part of the Healthy Weight Commitment Foundation removed 6.4 trillion calories from the food supply by the end of 2012, which equates to around 80 fewer calories per person per day, so that’s real progress.
The Partnership for a Healthier America has also made agreements with companies providing early care and education [such as Learning Care Group], although they still represent a minority of early care and education centers.
FNU: Should state or federal regulators tax soda or restrict portion sizes?
WD: Yes, even though the Bloomberg initiative [to curb portion sizes of soda in some outlets] failed, it changed people’s attitudes. That’s also a side benefit of taxes, because people are suddenly made aware of the issue, and even where they don’t pass, the message is getting through that sugar drinks contribute to adverse health effects.
Ultimately we all make our own decisions about what to eat and drink, but these decisions occur in a broader context. In some places, most of your food options might be in corner stores where sugary drinks cost less than anywhere else, for example, so if people pick them for their children, you could argue that it’s a rational choice based on their living circumstances, even if it’s not the right choice.
Things like menu labeling and the new Nutrition Facts panel are all steps in the right direction as well. Obama did more than any administration since Nixon’s to improve the health of children through federal programs.

Dr William (Bill) Dietz is the director of the Sumner M. Redstone Global Center for Prevention and Wellness at the Milken Institute School of Public Health at George Washington University, and a former director of the Division of Nutrition, Physical Activity, and Obesity at the Centers for Disease Control (CDC).
Get more CDC data HERE and read more from the Trust for America's Health and the Robert Wood Johnson Foundation HERE.
Read the latest CDC data on adult obesity rates HERE (released today).
